Abstract
Introduction: Cytokine Release Syndrome (CRS) is a systemic inflammatory response síndrome related to aberrant immune activation or immune hyperstimulation, leading to elevated cytokine levels (including IL-6, interferon-γ, IL-2) and inflammation. CRS has been described after infusion of T-repleted haploidentical progenitors in post-transplant cyclophosphamide (PTCy) based conditioning regimens. We analyzed the outcomes of 144 T cell-repleted transplants with PTCy (days +3, +4), MMF and CsA as GVHD prophylaxis in our institution.
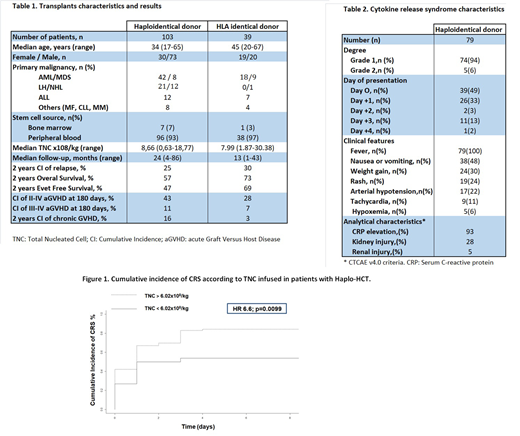
Patients and methods: A total of 105 haplo-HSCT and 39 HLA-identical HSCT (19 and 20 from sibling and unrelated donor, respectively) with PTCy were analyzed retrospectively in 141 consecutive patients from 2010 to 2017. Two patients with haplo-HSCT were excluded, one due to early death on day +1 and other for lack of information.
CRS was defined and graduated according to Lee et al. criteria published in 2014.1
Chi-squared test was used to study the association of different qualitative clinical variables and CRS and Mann-Whitney U test for the association between CRS and total nucleated cells (TNC) infused. The determination of the best cut-off of TNC to stratify patients with CRS was performed with ROC curves. The stadistical program used was R v2.15.0.
Results: The characteristics of the 142 transplants analyzed are shown in Table 1. CRS occurred in 77% of haplo-HSCT (79/103) and in 18% of identical HSCT (7/39). Most patients with CRS presented sings and symptoms in the first 24 hours after the infusión.The majority was grade 1. Only 5 patients who underwent haplo-HCT showed grade 2 CRS. They needed vasoactive drug, oxygen therapy (without mechanical ventilation) and low doses of corticosteroids. Of those 5 patients, 4 were lymphomas with a previous autologous transplant. The stem cell source of the 5 patients was peripheral blood (PB). We did not have cases of grades 3-4 CRS. No patient required Tocilizumab. The clinical and analytical characteristics of CRS are shown in Table 2.
In the univariate analysis, the use of PB was significantly associated with the development of CRS (p = 0.001). No statistical association was found with other variables (underlying disease, disease status, cryopreserved product, previous autologous or allogeneic transplant, conditioning, age, sex, CD34 infused, etc.).
In the haplo-HSCT cohort, patients who presented CRS showed higher content of TNC infused (median (range): 9.1 (1.17-18.77) vs. 6.9 (0.63-26) x108 / kg, p = 0.023). The best cut-off of TNC calculated was 6.02 x108 / kg (S 82%, E 47%, p = 0.02).CI of CRS in patients with TNC greater than 6.02x108 / kg was 84% compared to 53% in lower (HR 6.6, p = 0.0099, Figure1).
Patients with CRS developed grade II-IV acute GVHD more frequently than those who did not present CRS (60% vs. 28.6%, p = 0.012). No association was observed between CRS and chronic GVHD, relapse, non relapse mortality, overal survival or event free survival.
Conclusion: CRS appears more frequently in patients with haplo-HSCT compared to HLA-identical donors using PTCy and PB as stem cell source. In our experience, cases with grades 3-4 CRS are infrequent. The majority of CRS cases remit after PTCy and progress well with symptomatic treatment. In the haplo-HSCT cohort, the number of cells infused is associated with higher incidence of CRS and with the presentation of EICRa grade II-IV.
Lee DW, Gardner R, Porter DL, et al. Current concepts in the diagnosis and management of cytokine release syndrome How I Treat Current concepts in the diagnosis and management of cytokine release syndrome. Blood. 2014; 124(2):188-195. DOI: 10.1182/blood-2014-05-552729
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal